Family Medicine Advocacy Rounds, September 2023
AAFP works for congressional support for Medicare add-on code, access to new COVID-19 vaccines, and more
By AAFP’s Federal Advocacy Team
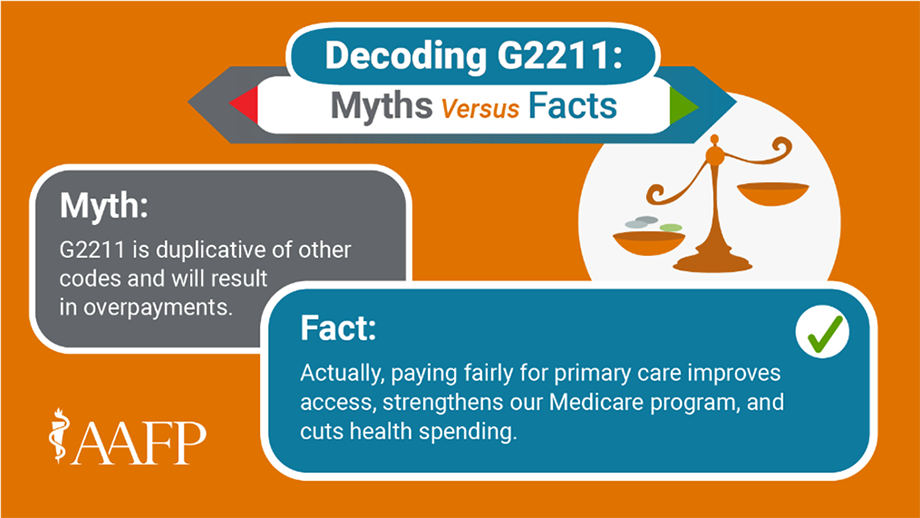
Family physicians continue to support G2211 add-on code
Why it matters:
Primary care visits are thoughtful, complex, and all about ensuring patients’ health care needs are met. Here's the catch, though: All that work physicians do isn’t appropriately paid for.
One Medicare physician billing code — set to go into full effect in 2024 — is specifically designed to pay more accurately for the complex, high-value visits that primary care physicians provide as part of a continuous relationship with a patient. The equation is simple. Better payment equals better patient access and better outcomes. G2211 can make this a reality.
Unfortunately, this important policy advance, poised to improve health care nationwide, has attracted opposition. But the misperceptions driving criticism of G2211 do not stand up to scrutiny.
What we’re working on:
- AAFP and 36 other health organizations representing millions of clinicians, patients, and key members of the health care community, have joined together to urge Congress to support comprehensive primary care and the implementation of the G2211 code in 2024 to bolster the health care workforce and safeguard Medicare beneficiaries’ access to high-quality, patient-centered care.
- The letter follows AAFP’s comments on the 2024 Medicare physician fee schedule proposed rule, which applauds the Centers for Medicare and Medicaid Services for advancing several proposals to support primary care. In addition to promptly implementing G2211, this includes new coding and payment for screening and addressing unmet social needs, and more accurate payment for behavioral health integration.
- AAFP and the American College of Physicians sent a joint letter to Congress on the need to support full implementation of G2211 in 2024. The letter stressed that G2211 will:
- Sustain primary care and other physician practices Medicare beneficiaries rely on and bolster the physician workforce,
- Bolster the physician workforce,
- Appropriately value primary care and other longitudinal, continuous care under the MPFS, and
- Ensure the Medicare program provides patients with timely access to comprehensive, longitudinal care.
- AAFP continues to call on Congress to end unsustainable physician payment cuts, reform arbitrary Medicare budget neutrality requirements, and invest in community-based primary care. Learn more facts about G2211 here.
AAFP comments on commercial transition of COVID-19 vaccines
Why it matters:
AAFP recently sent a letter to the U.S. Department of Health and Human Services with recommendations for facilitating access to new COVID-19 vaccines from trusted primary care physicians this fall. With COVID-19 cases rising, and because the transition of COVID-19 vaccines to the commercial market could create challenges for physician practices, we urge the administration to take action that will enable family physicians to support the fall COVID-19 vaccine campaign.
What we’re working on:
- AAFP's letter to HHS recommends:
- Setting appropriate payment rates for vaccines, vaccine administration, and counseling;
- Encouraging manufacturers to set flexible invoicing and buyback policies that will enable physician practices to provide COVID-19 vaccines in-office;
- Publishing a searchable list of sites for the Bridge Access Program (which is intended to provide vaccine access to the uninsured) on vaccines.gov while prioritizing contracting efforts with FQHC sites; and
- Providing guidance to state Medicaid officials with suggestions to ensure that Medicaid payment rates for vaccines and vaccine administration promote access for Medicaid and CHIP beneficiaries.
AAFP also requested relaxed policies in the Vaccines for Children program to address storage and operational challenges associated with participating in the program.
House of medicine united in reaffirming workforce priorities
Why it matters:
The physician shortage is a complex issue affected by growing demand, a history of underinvestment in primary care, an aging physician workforce, and economic pressures on the rural health system.
The U.S. faces a projected physician shortage of up to 124,000 physicians by 2034, with demand for physicians outpacing supply, according to the Association of American Medical Colleges. Further, the Health Resources and Services Administration estimates that, by 2025, there will be a shortage of more than 250,000 mental health professionals, including psychiatrists.
For physicians — in communities both urban and rural, in hospitals, clinics, and independent practices—a workforce shortage contributes to burnout, inability to take on new patients, shortened visit times, financial challenges, and increased administrative burden.
AAFP has consistently advocated in support of federal policies to address the shortage and maldistribution of adult and pediatric primary care, psychiatric, and other high-need specialties.
What we’re working on:
- AAFP supports the bipartisan Lower Costs, More Transparency Act, which includes reauthorization for seven years of the Teaching Health Center Graduate Medical Education program and will ensure that Medicare and its beneficiaries are paying the same rates for physician-administered drugs in off-campus hospital outpatient departments as they do in physician offices.
- AAFP and the American Academy of Pediatrics, the American College of Obstetricians and Gynecologists, the American College of Physicians, the American Osteopathic Association, and the American Psychiatric Association sent a joint letter to Congress urging investment in a strong primary care workforce and enactment of policies including:
- The Conrad State 30 and Physician Access Reauthorization Act, which allows physicians who complete their residency in the U.S. to waive the requirement to return home for two years if they agree to practice in an underserved area for three years;
- Long-term reauthorization of the THCGME program or the Doctors of Community (DOC) Act; the THCGME program helps to attract and retain physicians in rural and medically underserved communities while addressing the issue of physician maldistribution;
- The Mental Health Professionals Workforce Shortage Loan Repayment Act of 2023, which would make mental health practitioners eligible for the loan repayment program passed in the SUPPORT Act five years ago;
- The Resident Education Deferred Interest (REDI) Act, which would allow borrowers to qualify for interest-free deferment on their student loans while in a medical or dental internship or residency program; and
- The Rural Physician Workforce Production Act, which would lift the current cap on Medicare reimbursement payments to rural hospitals that cover the cost of taking on residents, to alleviate the disadvantage that rural hospitals face when recruiting new medical professionals.
AAFP weighs in on telehealth prescribing of controlled substances
Why it matters:
Millions of patients live in health shortage areas and face months-long waits for an in-person appointment, leaving them reliant on telehealth appointments to access care. That’s why the AAFP recommends permanent telehealth prescribing regulations that prioritize established patient-physician relationships while facilitating equitable access to care for our patients.
AAFP Board Chair Sterling Ransone, M.D., participated in a public listening session with the Drug Enforcement Agency to discuss telehealth prescribing of controlled substances. In the session, Ransone reiterated the AAFP’s recommendations that the DEA should not impose additional telehealth prescribing restrictions for controlled substances on physicians who have already established a patient relationship through an in-person visit.
What we’re working on:
- AAFP recently provided comprehensive comments, sharing support for guardrails that protect the patient-physician relationship and patient safety but also raising concerns about how the rules could result in significant burden and strain for both patients and physician practices.
- AAFP recommends that the DEA permanently allow telehealth-only prescribing of buprenorphine for the treatment of opioid use disorder.
- AAFP opposes discrimination against patients receiving sexually transmitted infection specific therapies, such as PrEP and PEP for HIV, in obtaining health-related services and life, health, or disability insurance. We also recognize the need for continued public and professional education about STIs, with an emphasis on prevention.
For the latest policy updates impacting family medicine, follow us at @aafp_advocacy.